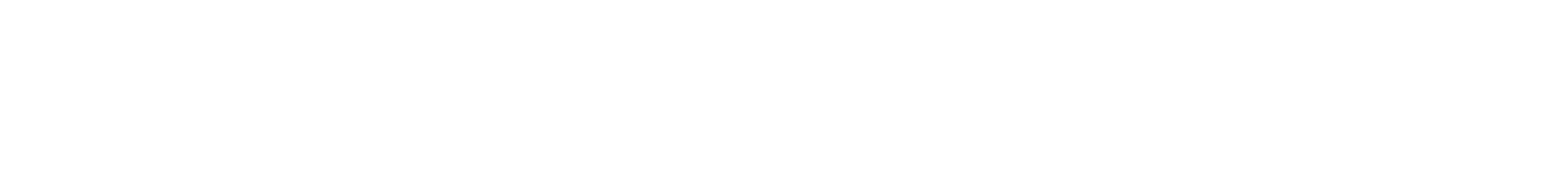
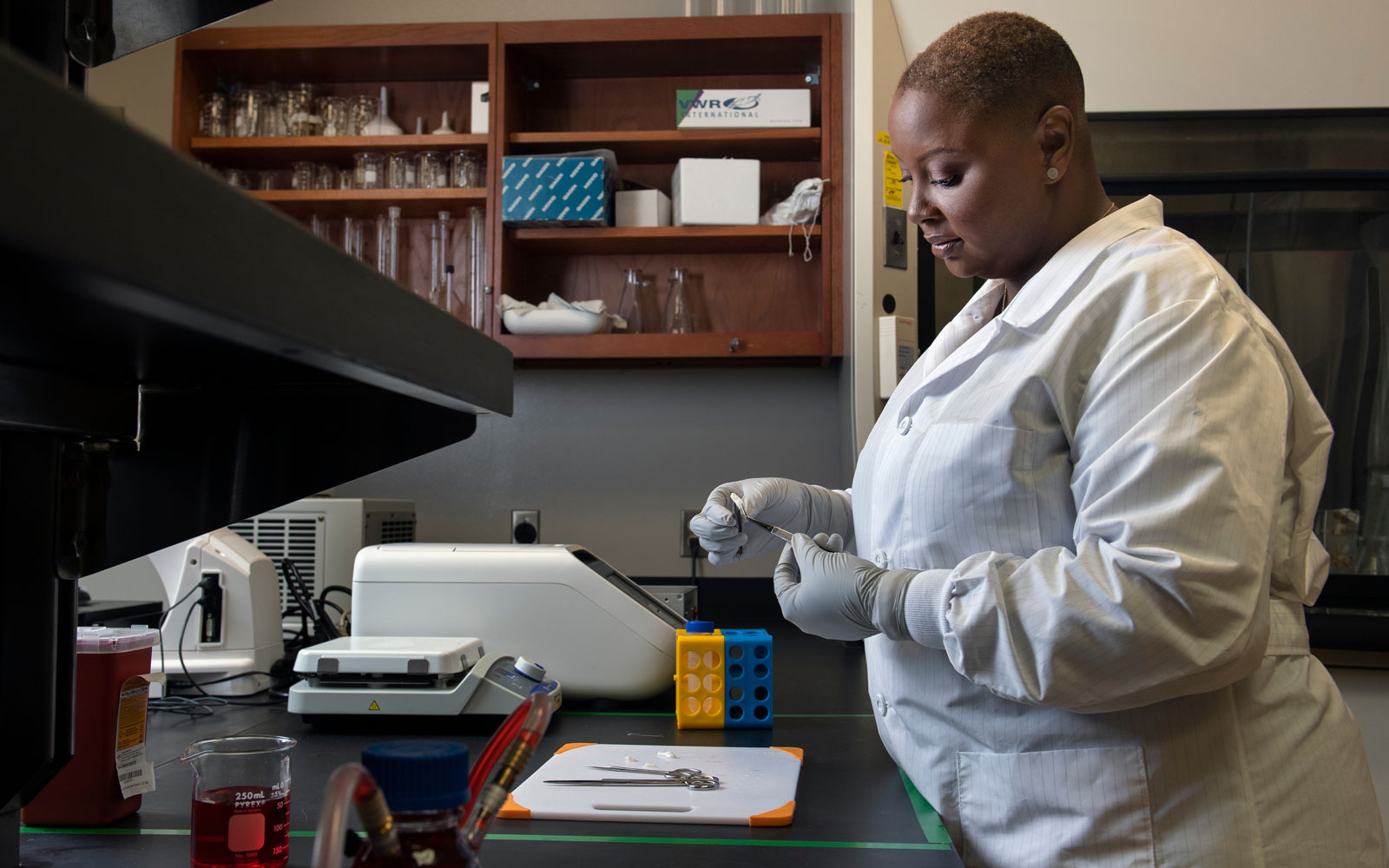
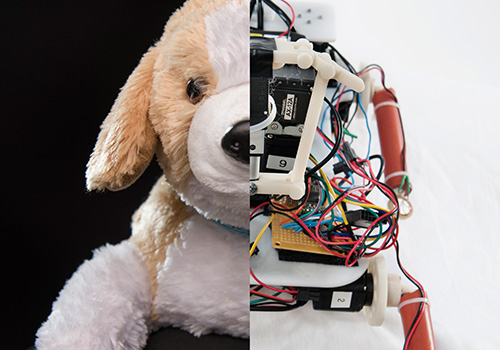
The purpose of the three-dimensional model is to show how arteries act differently inside the human body.
“Showing that we can induce calcification in a 3D model is important because it is more like what happens in the body where arteries are in a three-dimensional matrix, under flow all the time, in a soft material,” Simpson says. “This allows us to study healthy and diseased cells in an environment similar to the body, so we can solve the mystery of why and when smooth muscle cells make the switch to bonelike cells during calcification.”
From there, other types of cells that play a role in calcification can be studied and treatment options can be explored.